When it comes to gaining coverage for a Laboratory Developed Test (LDT), insurance companies are not the enemy. Payers are willing to cover and reimburse for an LDT that is clinically relevant, improves patient outcomes and hopefully reduces healthcare spend. So, what gets in the way of a laboratory achieving clinical relevance for their new tests?
Clinical Utility and Health Economics 101
New diagnostic tests are developed by laboratories to address unmet needs in patient healthcare. Intended for a specific audience and use, the performance of these tests must be validated to demonstrate a clinically relevant impact on the treatment decision, confirmation it was the right decision and an improved patient outcome. Also important are quantified health economics which either hold a payer’s cost curve, or preferably, improve it. If results provide positive impact on treatment decisions through improved patient outcomes and health economics, insurance companies are likely to consider coverage options. The burden is on the laboratory to establish this evidence.
Clinical Relevance Defined
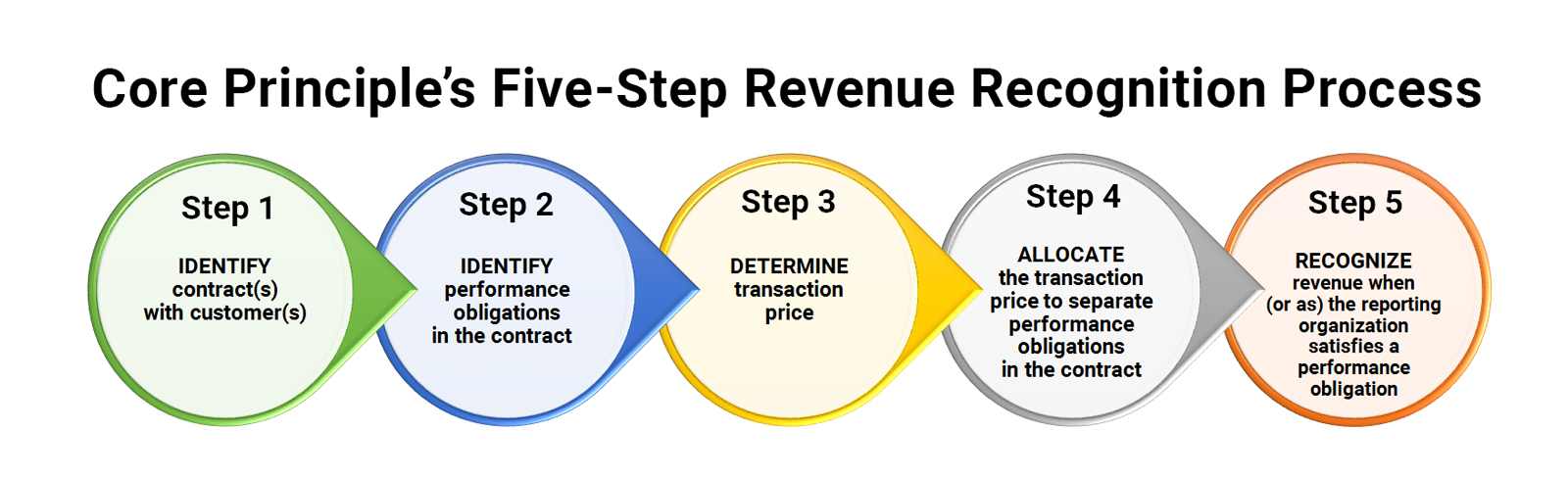
The collective goal is to improve upon the standard of care and patient outcomes. It all starts with the lab test’s ability to accurately and reliably measure what it was designed to measure. The measurement is then used to predict outcomes for a specific patient population within a well-defined, intended use. An LDT becomes useful when it provides new, relevant information to confirm or impact a treatment decision. When the treatment decision produces an improved patient outcome, the benefit can then be valued using a health economics model. Using this model, it is possible to demonstrate the lab test’s economic impact on the intended patient population. When a lab properly establishes clinical relevance, it can influence and assist in gaining payer coverage for the lab’s new diagnostic test.
What Gets In the Way of Demonstrating Clinical Relevance and Obtaining Coverage?
A laboratory must be aligned internally when seeking coverage and reimbursement for an LDT. Investors and senior management may focus too early on driving revenue, versus evidence development, on an overly aggressive timeline. When launching an LDT, a lab’s marketing team may want to promote to a broad audience which often leads to inappropriate use. In its pursuit of growth and volume, a company may hire a large sales team to drive utilization well before the evidence is ready to support broad coverage and reimbursement. These approaches have unintentional consequences of high costs and minimal revenue. As a result, demonstrating clinical relevance suffers and insurance companies choose to either not cover the test or cover with many restrictions and at a sub-optimal rate.
Where can your lab go for help?
Pursuing payer coverage requires continuous alignment and commitment to demonstrate clinical relevance at a value-based price. It can and will take years to achieve, but it can be done with a well-defined strategy and execution to develop the necessary evidence while supporting a controlled commercial launch.
Quadax provides a lab-centric revenue cycle solution. From patient advocacy and payer management to claims and remittance management, Quadax software, service, and support is sized to fit your lab’s needs. While your lab is working to establish clinical relevance and utility, our appeals strategy to increase revenue and decrease denials can help you defend the payments you deserve, get ahead of changing payer requirements, and influence payers toward ongoing acceptance of your tests.
An effective appeals strategy, run concurrently with both traditional and innovative evidence development, can help drive private payer coverage. For information and discussion on strategy design, register for the Q1 pre-show webinar Leveraging an Effective Appeals Strategy for Private Payer Coverage presented by Gordon Brown on February 1 at 10:00 a.m. EST.